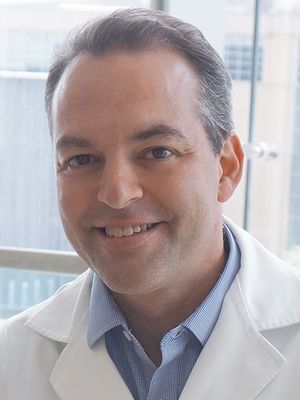
Philip J. Horner, PhD
Scientific Director, Center for Neuroregeneration;
Co-Director of Center for Regenerative and Restorative Neurosurgery;
Vice Chairman, Research, Department of Neurosurgery;
Professor and Full Member of Research Institute, Houston Methodist Neurological Institute
Abstract
Rewiring the Spinal Cord: Progress Toward Functional Circuit Replacement
In the early 1900’s Jorge Francisco Tello grafted a peripheral nerve onto the spinal cord discovering that the adult neurons were indeed capable of regrowth. Tello’s observation inspired more than a century of discovery focused on rewiring damaged spinal circuitry. A lofty goal has been the search for a neural ‘substrate’ or relay that can be safely placed within injured spinal cord tissue. Work in neural transplantation formed the bulk of promising discoveries, taking immature spinal tissue and developing the methods to transplant and grow new tissue within an injury environment. Despite exciting progress and eventual clinical trials, these approaches did not lead to significant circuit reconstruction or improvement in motor function. Nevertheless, this research laid the groundwork for feasibility and established the safety of surgically placing tissues and materials into an injured spinal cord. During the 1990s, often called the “Decade of the Brain,” researchers uncovered the basic molecular building blocks of the nervous system. Today, scientists can create nearly any type of spinal cord nerve cell from human cells in the laboratory. This powerful capability allows researchers to better understand spinal cord function and to test new repair strategies in ways that were once impossible. Progress in spinal cord repair is now accelerating, though it has become increasingly complex and resource intensive. Combined technologies of engineered human spinal circuitry, bioresorbable materials that can conduct electrical currents and advanced tools to re-awaken and stimulate damaged spinal circuitry are being combined to offer the realization of significant functional return in pre-clinical models. With focused energy and resources, spinal cord circuit replacement and the clinical reversal of paralysis is an eventuality and no longer a dream.
Bio
Philip J. Horner, PhD is the Scientific Director of the Center for Neuroregeneration, Co-Director of Center for Regenerative and Restorative Neurosurgery, Vice Chairman, Research, Department of Neurosurgery, Professor and Full Member of Research Institute with Houston Methodist Neurological Institute. Dr. Horner is a member of the Program in Neuroscience at Weill Cornell Graduate School and is co-Director of NeuralCODR Post-Doctoral Training Program at Houston Methodist Research Institute. Dr. Horner is a member of the HMAI President’s Council and serves as Chief of Graduate Studies. Dr. Horner received a Ph.D. in physiology from Ohio State University in 1995. He did post-doctoral training with Dr. Fred H. Gage and became a staff scientist in the Lab of Genetics at the Salk Institute in 1998. In 2001, Dr. Horner joined the faculty of the Department of Neurological Surgery at the University of Washington in Seattle. He directed a laboratory at the UW South Lake Union Campus and was a member of the Institute for Stem Cell and Regenerative Medicine. Dr. Horner was a Christopher Reeve Fellow from 1997-2001, received a EUREKA R01 Award from the National Institutes of Health in 2009 and was selected as the 2021 G. Heiner Sell Lecturer by the American Spinal Injury Association. Dr. Horner’s research spans pre-clinical models through human studies. Dr. Horner holds patents on devices for promoting regeneration and repair as well as imaging methods for detection of damaged nerve fibers in the injured nervous system. Dr. Horner’s research focuses on the role of glial and neural progenitor cells in the regeneration of the injured and aging nervous system.