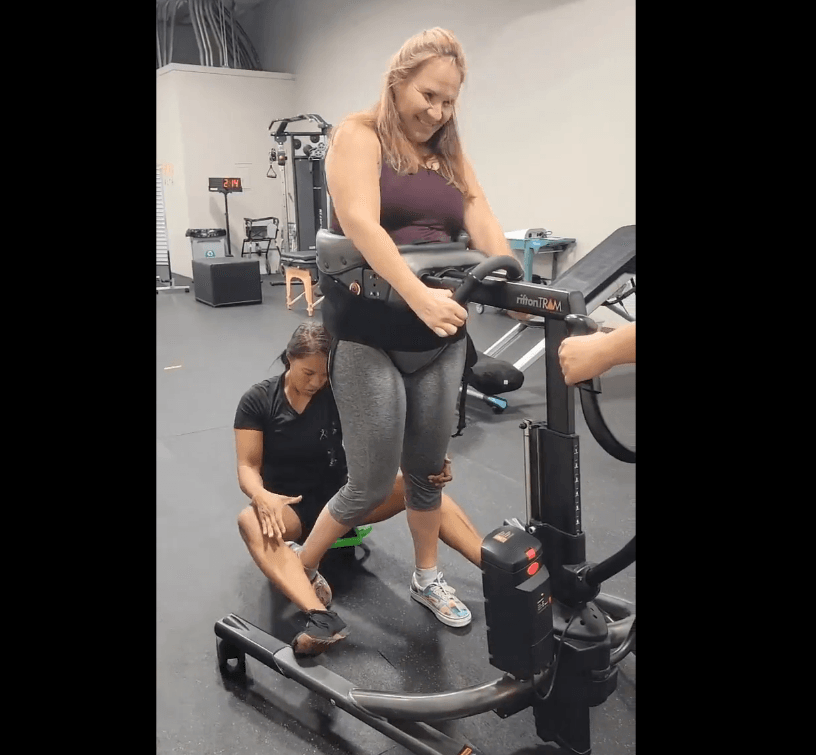
Above: Laura Grabowski (C7) working with one of her PTs at Reneu Health had a spinal cord stimulator clinically implanted by Uzma Samadani earlier this year
There’s wind in the sails of neuromodulation. It’s not news that a few dozen people with spinal cord injuries have gotten stimulator implants, in clinical trials and more recently in a Minneapolis clinic. Nearly all of them report meaningful recovery.
So here’s today’s stitch: pull any thread of this story, and it always comes back to U2FP. Try it. We are in this recovery of function business at a very deep level.
Before meeting some recent stim recipients and their optimizers, this is necessary backstory: Three doctors from the University of Minnesota - David Darrow, Ann Parr and Uzma Samadani - got a grant from a new state program to fund SCI research. That funding was hammered through the Minnesota state legislature in 2015 by SCI citizen advocates, led by Matthew Rodreick, now executive director for U2FP.
None of what follows would have happened without the Minnesota state funding. Indeed, the advocates crafted the legislation so that grantees are chosen by an advisory board that includes SCI community members. If you want to read about U2FP’s efforts to create and maintain a $26 million funding stream for SCI research – in Minnesota, Pennsylvania, Ohio, Washington and (maybe, it’s looking good) Wisconsin - go here.
In 2017 these doctors used their grant money to start a clinical trial (it’s still recruiting) called E-STAND, to see how epidural stimulation worked without months of pre- and post-op physical therapy. It worked. Results have been published in medical journals and participants report a range of benefits, including blood pressure management, bowel and bladder improvement, sexual function recovery, overground walking, and volitional movement when the stim is off.
If neurosurgeon Uzma Samadani’s story isn’t familiar to you, please check out her presentation at the 2021 U2FP Symposium, or her interview on the CureCast podcast. You won’t find a more responsive, caring, patient-centric neurosurgeon. She fell in love with her specialty on the first day of medical school rotation. Said Samadani: “I saw it as a real opportunity to change people’s lives. I wanted to be able to do dramatic interventions. Neurosurgery is that. There’s a huge amount of job satisfaction – when you take out a tumor, for example. For SCI, and brain injury, though, there are very few options – it just breaks your heart. Why can’t I do anything?”
Samadani had patients that she thought might benefit from neuromodulation, but weren’t eligible for the clinical trial. “It doesn’t seem fair not to include people who might benefit but don’t fit the trial inclusion criteria. There are so few trials to begin with.” So, she said, let’s give it a go in my private practice clinic. And let’s get it paid for by insurance.
On-Label for Pain
Spinal cord stimulation (SCS) is a common procedure in neurosurgery; thousands of stim units are placed every year in people dealing with pain. You might hear the term off-label applied to Samadani’s approach – that’s when a doctor applies a treatment to a condition that the treatment was not approved for. SCS is approved for complex regional pain syndrome. “Almost anyone with a spinal cord injury has some amount of pain, of course,” said Samadani. The constellation of symptoms includes contractions, joint stiffness, swelling, muscle spasms, tremors and weakness. Samadani isn’t technically working off-label.
Samadani has done about two dozen SCS implants and has gotten each one paid for. The first were in the VA system. “We have also had patients get this paid for by BCBS and United Health Care,” she said.
I wondered if Samadani gets pushback for being a little hasty going to the clinic with epidural stim. No one has called her out, at least not to her face. “I am not a fringe person. But as a brown woman in the field of neurosurgery, I’ve gotten used to swimming against the tide.”
The real question may be, why aren’t more neurosurgeons doing this? “There are people talking about it,” said Samadani, “and I think it's definitely gaining momentum. This technology offers a huge opportunity – we have to help people; we have to do all we can. If a patient tells me he got his life back because of this device, well, that’s the point.”
SCS will be clinically approved at some point. Hopefully, doctors can better understand how different patients will respond to these devices, which is far from the let’s turn-it-on-and-see approach happening now. The functional benefits for spinal cord injured individuals will be directly proportional to the amount of post-surgical help patients get figuring out the millions of stim parameter options.
David Darrow, the principal investigator for the E-STAND trial, understands that SCS response must be customized for each patient. Just this week, he published a paper, Mapping Spinal Cord Stimulation-Evoked Muscle Responses in Patients With Chronic Spinal Cord Injury. Fifteen E-STAND participants were included. The variability in response to stimulation is surprisingly wide, Darrow said. “This means that personalization remains paramount for neuromodulation.”
Personalized optimization help is only now taking form. Darrow started a company, StimSherpa, to help people tune spinal cord stimulator software. That sort of platform is very much needed, but it’s not ready. The device companies will continue to play a role. Abbott, which makes the stimulators both E-STAND and Samadani use, has so far been very responsive to patient and therapist queries about settings and parameters. But as the deployment of these devices scales up, what can a company be counted on to do, once the device is paid for and implanted?
The therapist sector will be critical. U2FP is helping to create a network of activity-based therapy centers. Maybe they can form a stimulator optimization syndicate of sorts.
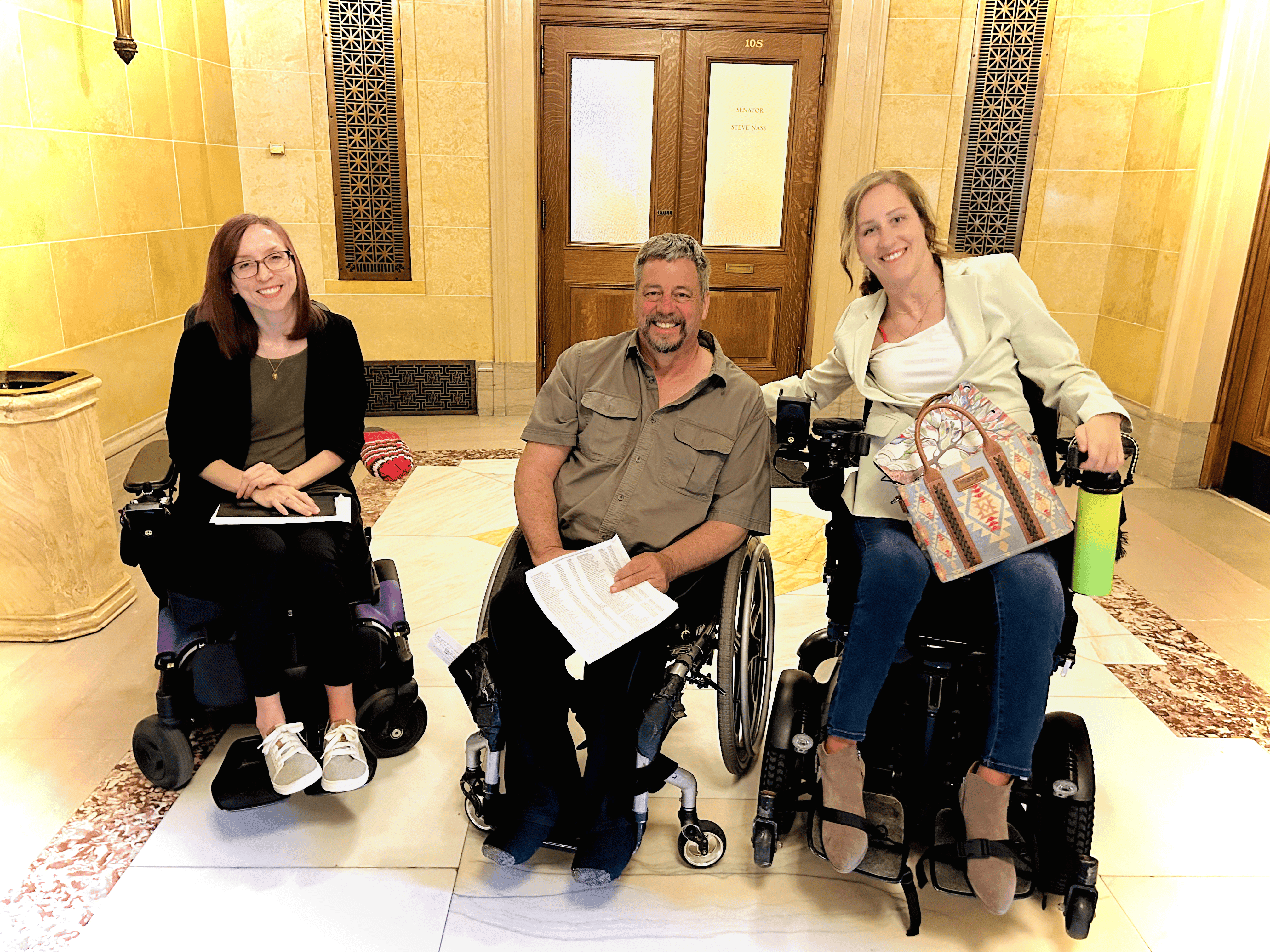
At this juncture, there are just three places Samadani can recommend to a patient to make sure their device settings are optimized for what that person wants from the stim. Two are activity-based centers: TryAbility, in the Chicago area, owned by U2FP board member Traci Fernandez; and Reneu Health, in Southern California, managed by U2FP board member Christel Mitrovich. The third setting is a VA physical therapy clinic in Minneapolis, where PTs Elizabeth Koch and Ann Goding have worked with at least six stim implant patients.
One of those Minneapolis VA patients is John Lee.
Suni Lee’s Dad
The Minneapolis media market hears about spinal cord stim more than most places, partly because of E-STAND and Samadani, but mainly because of their home girl, Olympic gymnast Suni Lee, who took Tokyo by storm in 2020 winning a gold medal in the individual all-around event. Her father, John, was spinal cord injured in 2019 and in 2021 was implanted with a spinal cord stimulator by Samadani. Local media has regularly featured his recovery – working with Koch and Goding, he uses an exoskeleton that magnifies his leg function. Last March, Lee could take 23 steps, ramping up to 633 in May and 1000 in November.
Lee’s goal is to fully regain walking function. That’s asking a lot of neuromodifying his AIS A (complete) spinal cord injury, but he’s continuing to improve in lower limb function, sleeps better and has better bladder capacity.
Samadani had this to say to a local reporter about Lee: "I think this is as close to a miracle as you can get in neurosurgery when you take someone who's paralyzed, and you get them to move again."
Motivated to Recover
In 2019, Laura Grabowski was paralyzed at C7 in a mountain bike mishap near her home in San Diego. A career in scientific research (cancer) led her to ponder the SCI recovery possibilities, soon leading her to U2FP. She had been in contact with executive director Rodreick about being part of their Lab Rats program -- being placed as a consultant in an SCI research lab (that will indeed happen early next year).
Grabowski knew about SCS and the E-STAND trial and was intrigued by the potential range of recovery, including sexual function by two women. Alas, she did not qualify for the trial. Grabowski said she had been approached by the University of Louisville about being part of the large epidural stimulation study there. She discussed this with Rodreick who told her that if she didn’t want to relocate to Kentucky, Samadani was doing spinal cord stim implants outside of E-STAND, in her clinic. Grabowski watched the video from the 2021 U2FP Science and Advocacy Symposium. She asked for an introduction to Uzma.
Grabowski visited Samadani in Minneapolis in July, and got screened for the study. Paperwork was filed with United Health, and to Grabowski’s shock, she didn’t have to put up any fight whatsoever to get her implant surgery fully covered. She had the stimulator surgery in September.
When the stimulator was first turned on, Grabowski could move a leg and initiate some hip flexion. She came home and knew she needed to work on tuning the device. Pre-surgery she had been working with San Diego sports trainer Eric Harness, a pioneer in activity based exercise for SCI, and with physical therapists from Reneu’s San Diego branch.
Christel Mitrovich, Reneu’s Director of Operations, has worked in activity-based exercise for 20 years and is quite familiar with neuromodulation. Her clinic is helping the company SpineX test its skin surface spinal cord stimulation device. She and her team recognize the unmet need in providing PT for post-implant patients. Said Mitrovich, “Dr. Samadani told us she needs groups like ours to report back to her about our clients’ outcomes and their various stim parameters. We see a real need ahead for our post-implant therapies.”
Trial and error, that’s how it is with optimizing stim devices. “We really had no idea what to do with dialing in the stim settings,” said Grabowski. She works with Harness once a week and with her PT at Reneu four days a week (not covered by insurance). Harness works more on individual movements; Reneu is helping Grabowski learn to stand and make a transfer pivot. She shared a recent video – she’s getting close to the standing part.
Would she do it again? “I would 100 percent recommend this,” Grabowski said. “But not if you do not have the support of someone who can help figure out the settings. On your own, it’s useless.”
That’s where Brad Baker is: On his own and feeling like his epidural stimulator is useless. He hasn’t even turned it on in a year.
Not Quite Magic, Bullet
Baker, nicknamed “the Bullet,” has been well known in the motorcycle community since he was a teenager. He was injured in 2018 at T6 (AIS B, has some sensation) at an X-Games flat-track qualifier race at the US Bank Stadium in Minneapolis. The hospital happens to be right across the street from the Hennepin County Hospital, where they took him after he got bucked off his bike. “I lucked out. If you’re going to break your back and get a spinal cord injury, I picked a good place to do it.”
Samadani was his attending neurosurgeon and did a decompression surgery. He completed his inpatient rehab at Shirley Ryan in Chicago and a few months later relocated from Washington State to Michigan (the family of his then girlfriend, now wife, is from there).
He stayed in touch with Samadani, who had him come back to Minneapolis in 2019 for an MRI and eval. She told him about her epidural stim work. He was interested, but didn’t meet the requirements for the E-STAND trial. She told him she could hook him up with a stimulator. Out of pocket, it would run him about $120,000. “I wasn’t going to pay that myself, not knowing if it would even work or not,” said Baker. So Uzma suggested they try to get it covered by his insurance. And so they did, after one denial, from United Health Care.
Baker got the implant two years ago this December. He went home to Michigan a week later, having had just two hours of stimulator programming from the tech from device maker Abbott. He had a handheld controller that could modify some settings, but after a lot of trial and error on his own, he gave up.
SCS failed to deal with his pain, and he experienced function-canceling episodes of co-contraction when trying to stand, pitting muscles against themselves, putting him on his tippy toes. The stim also didn’t work the same when he was standing as it did when his back was not straight.
Last week, Uzma checked in on Baker and heard his frustration. She thinks his device can be much better tuned to help him, but acknowledged it’s difficult to do this remotely. She recommended he get himself to the Chicago area to the TryAbility center. He’s considering it.
TryAbility owner Fernandez knew about Samadani’s work from her involvement with U2FP and wanted to see if she could participate. As with Baker and Grabowski, she didn’t qualify for the E-STAND trial. In her case, it’s because her paralysis is not trauma related. She woke up one day with pain, went to the hospital and could no longer walk – her transverse myelitis presents just like T4 paraplegia.
Fernandez had an epidural stim system implanted by Samadani a year ago. She got immediate relief from nerve pain and continues to experiment with stimulation settings to affect leg extensions. She’s happy with hers and if you get one, maybe she can help you get happy with yours.
Any way you weave it, the neuromod thread stitches back to U2FP. So thank you for your support, please help us move this technology forward with greater dispatch and urgency. Donate here.
Stay curious,