Memo to FDA from people living with spinal cord injuries: We respect your process for keeping a tight gate on safety and efficacy for new therapies and devices. Heed our voice: there is urgency. Please accelerate translation from research to clinic. And consider spinal cord injury not as a massive movement disorder or set of isolated conditions but as a whole-body disease state.
Unite 2 Fight Paralysis has participated in two recent meetings with the U.S. Food and Drug Administration (FDA). The regulatory agency is being urged to increase its awareness of spinal cord injury community needs, and to embrace new ways of assessing clinical trial results.
The first meeting was an FDA Listening Session organized by U2FP and included 42 FDA staff and seven individuals living with SCI. The goal was to help the agency better understand SCI and the priorities of patients, caregivers, and advocates. We asked the FDA to consider the benefits of broadening outcome measurements for clinical trials by reflecting a variety of possible clinical improvements within the small, diverse SCI community.
The second meeting was convened by the North American Spinal Cord Injury Consortium (NASCIC) with the FDA’s Center for Devices and Radiological Health (CDRH) office. This conference call included testimony from U2FP, Reeve Foundation, United Spinal and Conquer Paralysis Now. Testimony informed CDRH of NASCIC’s community engagement efforts within the SCI community and of the preferences and priorities of those living with the condition (see below).
Listen Up
The FDA hosts a Patient Listening Session once or twice a month, meeting with various patient groups representing rare or underrepresented conditions (see this list of recent Sessions).
Per the FDA, “Patient Listening Sessions help the agency inform medical product development, clinical trial design, patient preferences, and shape our regulatory thinking.” The Sessions are informal and non-regulatory. The FDA hopes to “better understand what is most important to different communities and individuals who have specific health, medical, and treatment needs.”
The SCI Listening Session was organized by Matthew Rodreick, Executive Director, U2FP. There were numerous pre-call planning meetings with the FDA’s Patient Affairs office over 9 months.
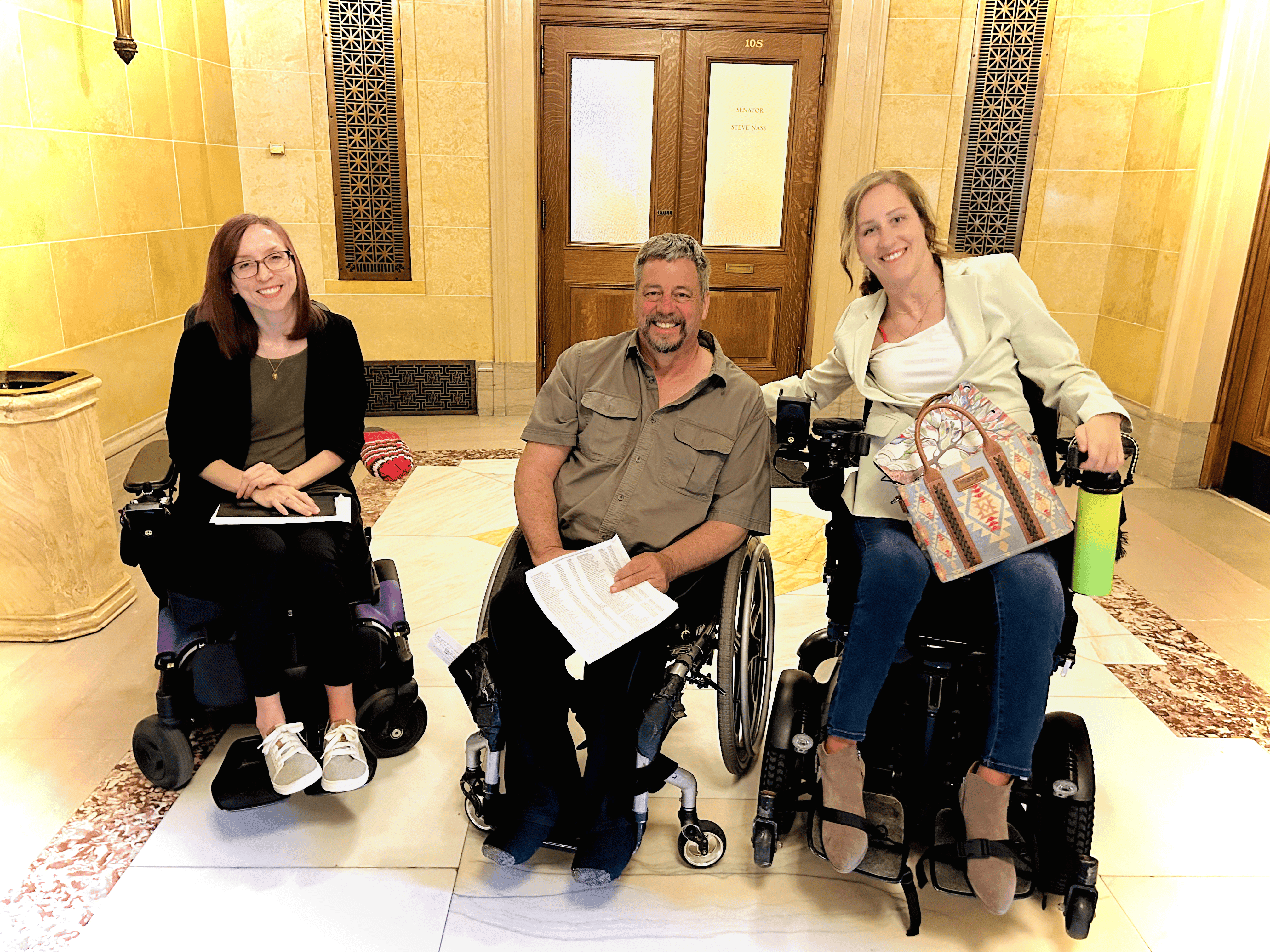
Other participants from U2FP included: Jason Stoffer, Co-Director for U2FP’s Cure Advocacy Network and co-host of the CureCast podcast; Jesus Centeno, quadriplegic, computer science student and CAN activist in Texas; Leon Ford, paraplegic advocate from Pittsburgh; Allie Leatherman, quadriplegic and CAN activist in Ohio; Traci Fernandez, paraplegic from the Chicago area and U2FP Board Member; Kent New, quadriplegic and physician/scientist in Florida; and Quinn Brett, paraplegic and U2FP Board Member from Estes Park, Colorado. They shared their injury story, details of day-to-day struggles with SCI, what they would like to see in new therapies, and what degree of risk they would be willing to accept in a clinical trial.
The FDA listeners included staff from the Patient Affairs office, representatives of three divisions of the Office of the Commissioner, four divisions of The Center for Biologics Evaluation and Research, seven divisions of the Center for Drug Evaluation and Research and from 11 divisions of the Center for Devices and Radiological Health (CDRH).
How U2FP Set This Up
From Rodreick:
What we proposed to the FDA is something they generally don’t hear from patient groups. The FDA usually hears about how a disease or condition is difficult and needs a treatment. We were more strategic. We wanted them to hear about the difficulties of living with SCI and the many complications that have nothing to do with walking. But we also asked them to consider looking anew at how outcome measures are used in SCI clinical trials. Usually there is one or maybe two outcomes -- for example the tested drug or device might address spasticity or hand function. What if it also has an effect on pain for some people? Our point was that by limiting an application to a small slice of its potential makes things even harder -- by sifting out a smaller outcome sample in an already small market.
Rodreick urged the FDA to understand SCI as a whole-body condition, to categorize it as a disease that includes many complications, for example pain, spasticity, autonomic dysreflexia, and movement disorders.
The FDA will say ‘it’s industry that picks the outcome measure for clinical trials.’ Then industry says the FDA only wants one primary outcome. My thought is, how can we disrupt that. So, let’s say the company Onward has picked cardiovascular function as its primary outcome for epidural stimulation. We know this stim affects many other things – movement, pain, bladder, sexual function, etc. What if the outcome measure could be any or all these things? Our concern is that once an outcome is approved it will take forever for all the other benefits to get approved.
Testimony to the Listening Session
Kent New is an MD/PhD who practiced neurosurgery for nine years prior to a C6 SCI in 2014. He described his experience as a reviewer for FDA’s Orthopedic and Neurological device group, his own participation in an FDA approved stem cell clinical trial, and of his continuing involvement with clinical trials for devices.
Despite my background as a clinician treating patients with neurological conditions, I am here today as a patient. I can tell you with more certainty than almost anyone that spinal cord injuries are poorly understood even by the majority of physicians involved in their treatment. They just don’t understand the day-to-day, life-altering impact of these injuries. In fact, I believe that after today’s Listening Session you will have a better understanding of the concerns of most patients with SCI than the majority of physicians.
So, what is an effective treatment for patients with SCI? Before I was injured, I thought an “effective” treatment for SCI would have to get patients walking again. Now that I have an injury myself, I realize how mistaken I was. There is so much more to SCI that affects quality of life. The reality is that patients with SCI want any treatment that can improve their quality of life. This includes walking but more importantly for most patients improving bowel/bladder function, sexual function, hand function (in cervical injuries), and autonomic function would have a very positive impact on their lives.
For me personally, I would undergo any treatment that would improve my level of independence; including improved hand function, ability to stand with or without assistance, regardless of ability to ambulate, improved blood pressure control or temperature regulation. I never thought much about the loss of autonomic function before my injury, but I can tell you now that low blood pressure and poor temperature regulation have a significant impact on my quality of life every day.
New described the issues for bringing effective treatments to patients.
I think the fact that no treatment is yet available for SCI despite the promise of interventions seen over the past 10 years is an indication that our system is not working well. I don’t know all the answers on how to fix it. I’m just suffering from the impact of the injury like thousands of others.
You may be thinking, well treatments are definitely needed but they’re not available because SCIs are so difficult to treat. But in fact, a treatment is out there in investigational studies that has benefited patients with several of the symptoms I mentioned for over 10 years now. I think we all need to ask ourselves, why isn’t this treatment widely available? Why hasn’t a sponsor brought this treatment to the FDA for approval yet?
New is talking about neuromodulation, a broad therapy that offers different benefits to different patients. This technology is central to the single outcome discussion – say the approval for blood pressure management is done, where does that leave people who respond with bladder improvement, or movement? Why not include them all as a clinical trial outcome?
Said New, “Industry sponsors have to pick one primary outcome measure in clinical trials. The majority of SCI patients would take any improvement in a number of various symptoms of their injury.”
New suggested the FDA could speed translation by changing its approach to approving therapies based on safety first. “Phase 2 clinical trial data, which generally strongly supports safety and has at least some reasonable support of efficacy, could and should be used to grant approval without completion of a large Phase 3 trial in certain cases, taking into account the severity of the condition being treated. In my opinion, approval of treatments for terminal conditions and permanent injuries should be based almost entirely on safety.”
Jason Stoffer urged the FDA listeners to up the ante on urgency. “Just because spinal cord injury is not ‘terminal,’ there is an everyday death - not just the ten years less of life expectancy, but also the opportunities lost.”
“People living with paralysis have to play the game of rating which functions we want back the most,” said Stoffer.
Allie Leatherman has a cervical injury and lacks hand function. A big part of the condition is mental. “The dark days still come, nine years out from my injury. Sometimes it cripples me all over again thinking about the things I can’t do, the lack of independence, the lack of empathy from people I know.”
Quinn Brett, a professional climber injured from a fall, testified that “Spinal cord injury is relentless.” She doesn’t expect to run up a mountain again, but she’d love to stand and hug someone, and be able to pick something up from a high shelf.
Jesus Centeno was injured at C6/7 when he was 11. He can move his hands and wrists but not his fingers.
I still remember hearing the words that the doctors told me that I would never ever walk again! Hearing these words over and over again really just made me depressed and not want to live. Thankfully though through my family I have managed not to give up on life and I'm still here fighting even after so many years. I'm still hopeful though that one day we will find a cure for spinal cord injuries and I will be able to get out of this wheelchair and walk again. I've come to realize that I don't really care if I don't ever walk again. If I can have control over my bladder and bowel that would be amazing. It would also be good to have my sexual function back.
Traci Fernandez has transverse myelitis, the kind of spinal cord disease wherein you suddenly wake up one morning paralyzed. “SCI impacts everything and everyone around you. Every step of your day. You go from helping people around you, to constantly having to ask for help. It is tiring for people around you. Most marriages dissolve in this situation. You can’t go to your friends' houses. You can’t ride in someone’s car. Non-stop constant planning of everything you do every day.”
Fernandez has participated in clinical trials, has an epidural stimulator implanted on her spinal cord, and is currently running a trial testing skin-surface spinal cord stimulation. Regarding the focus on a single outcome, she noted that in her stim patients, the stated outcome goal is hand function.The device, however, is applicable for many other uses including breathing recovery, lower extremity movement, etc.
How Much Risk
One of the FDA listeners asked the SCI group how much risk they'll be willing to take in a clinical trial. Several have already been in clinical trials and would consider participating in another. Leatherman and New were among the handful of chronic SCI participants in a 2014 neural cell transplant study from a company called Stem Cells, Inc. While early data indicated a meaningful effect on hand function, the company abandoned the trial a few months later. Leatherman said the experience “was terrifying.” She actually lost function, but said she’d still be interested in participating in future trials.
New said risk is not a big issue. “Trials don’t get much riskier than the Stem Cells, Inc. one, and they didn’t have any trouble recruiting people. No trial with any promise will have trouble recruiting patients because of the risks involved.”
Fernandez said people are eager to join trials: “We needed 20 people to sign up, but have a waiting list of 32. Patients would take an exorbitant amount of risk just to try to get help.
When his son, Gabriel, was first injured, Rodreick took him to India for five months for stem cell treatments. Gabriel regained a bit of function, perhaps due to the cells. Rodreick still fields calls from people asking if they should go abroad for treatment. “There is a desperation, especially early on in injury, there is a powerful appetite for regaining independence, and therefore a lot of willingness to take risks.”
NASCIC meeting
The second meeting between FDA and the SCI community was organized by NASCIC and held several weeks after the U2FP Listening Session. There were two components:
- SCI community engagement and preferences, with comments from Jennifer French, NASCIC president, Barry Munro, NASCIC treasurer and U2FP Board Member, and Kim Anderson, SCI researcher who lives with SCI.
- Discussion from people with SCI lived experience, including facilitator Ian Burkhart (C5), Rex Marco (C3), spinal surgeon, representing Christopher and Dana Reeve Foundation; Tiera McQuater (C3), Board Member, Conquer Paralysis Now; Matt Castelluccio (C6), Director of Community Support, United Spinal Association; and Jason Stoffer (L1), Cure Advocacy Network Manager, U2FP.
The following summary of the group discussion was provided by NASCIC:
- Q: In your experience and as a leader in the community, can you describe what you view as what would be a meaningful improvement?
Any improvement gives hope. There is heterogeneity in the community. Anything that increases independence, lifespan, and overall health. Anything that provides a better quality of life from access and/or functional ability.
- Q: Viewing the clinical trial (CT) barriers/facilitators, what other barriers have you seen hindering CT participation?
Common medications tend to be exclusion criteria. Eligibility requirements are a hurdle. Lack of awareness, financial considerations i.e. travel/accommodation/medical expenses. The opportunity cost to participation is a factor, plus weighing the medications and QOL.
- Q: What perspectives have you seen as the diversity between various levels of injury?
Higher-level injuries (tetraplegics) have a greater interest in clinical trials and gaining function back. In contrast, those with lower-level injuries are more interested in quality-of-life improvements of secondary complications for day-to-day life. We tend to avoid the word cure and focus on more attainable gains, but we can’t forget there is still a desire for a cure.
- Q: Could you talk about what you have seen to help serve minority, under-served, and rural area people with SCI?
Rural access is limited since most studies are conducted in urban centers. Whether it is the level of injury or time post injury, people are cautious due to a fear of lost function. Time commitment is another factor. Time since injury has an impact on interest.
- Q: How do you think the FDA could do better? What would you change? Understanding (and applying) the diversity in the SCI community. The NASCIC course is a great resource to get someone started in understanding their injury and how the research system works.
- Q: Are there any particular aspects of the design of clinical studies (including informed consent forms) that the FDA could help to improve in our reviews? Informed consents can be very long and complicated. The FDA could encourage continual informed consent and continual understanding of the risks. Anything that allows for remote data collection would be helpful. Understanding of when is a good time to go over informed consent.
- Q: What are some innovative or creative ideas we could use to improve the safety of the use of devices that are already in use for people with SCI?
Accelerate translation. Minimize revision surgeries and have tools to troubleshoot or correct system issues externally rather than before considering surgery. We need better long-term data for implants and better device contingency plans for when companies go out of business or research ends.
- Q: How can we follow clinical trial participants with implanted devices to improve the devices long term?
We need to look at standards of care. There could be an improvement in the longevity of devices. FDA could set up a registry for those with implanted devices, regardless of how long the investigator conducts their study or when it goes to market. FDA has a database of adverse events and could learn from there to improve devices.
We’ll Stay in Touch, FDA
We are well aware that the process of getting a new drug or device from those who invented it to those who it must pass through the FDA. While the agency hasn’t had any recent SCI-related judgments to make, there are therapies moving toward the market, and thus into the complex FDA regulatory process. So, thank you FDA, for including people living with spinal cord injury in the discussion – the purpose of both the U2FP and NASCIC meetings – the agency is better prepared to gauge the urgency for new treatments.