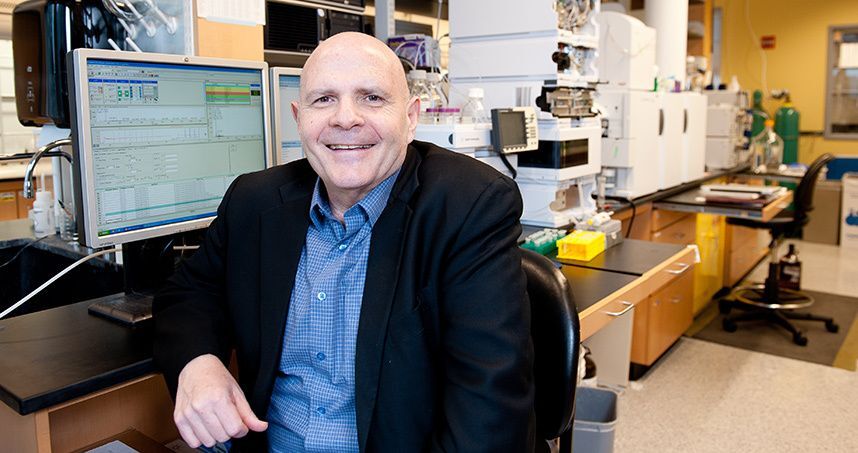
A year ago, Matthew and Jason interviewed Northwestern University scientist Samuel Stupp on U2FP’s CureCast podcast. Dr. Stupp had recently made mindstretching news by injecting paralyzed mice with a seeded liquid plastic scaffold (he called them “dancing molecules”). The real headline: animals recovered some lost function.
Stupp appeared at the U2FP Science and Advocacy Symposium last year in Salt Lake City. His presentation is not available in our archives but here’s a three-minute video from Northwestern describing the study. Also, see Stupp’s website for more.
CureCast reprised the original podcast, re-edited by producer Julie Censullo with improved sound quality. You can give it a listen here. I’ll provide some context for the nanotech scaffolds work, and also describe a brand-new paper from Stupp’s lab combining his dancing molecules with a type of stem cell made by genetically reverse-programming a human skin cell to become a neuron. That is what’s called an induced pluripotent stem cell (iPSC).
At the Molecular Hop
First, let’s refresh the molecules in motion. Stupp has worked on polymer scaffolds for 30-plus years and although the idea of nanomedicine is not new, this SCI related research seemed to come out of nowhere.
Stupp’s polymer is injected by syringe and then assembles itself into a tubular matrix. Bioactive chemicals can be attached to the matrix to trigger activity in the damaged spinal cord. The injected synthetic becomes a miniature, biodegradable, therapeutic scaffold. In this case, two biological signals were attached — one for laminin, which helps differentiate stem cells into neurons and promotes axon growth, and one for fibroblast growth factor 2, which activates a receptor to promote cell growth and survival. Once the regenerative cargo is offloaded, the polymer is absorbed in the body with no apparent side effects.
Per Stupp, his polymer improved spinal cord injury recovery in five ways: regenerating axons (nerve fibers); reducing scar tissue barriers to nerve growth; rebuilding myelin, the insulation of axons necessary for electrical efficiency; forming new blood vessels to nurture cells at the injury site; keeping more motor neurons (the ones delivering movement messages to muscle) alive after trauma.
So, first, keep in mind, this is an animal experiment in an acute injury model – it’s a long way from being clinical. Second, the science community is not all-aboard on the nanotech précis. Stupp gets pushback at science meetings from SCI specialists who study biology (Stupp is a materials scientist).
Nonetheless, the research is compelling, as noted by U2FP contributing writer Alina Garbuzov, a postdoctoral researcher at the University of California/San Diego, who also has a spinal cord injury. She covered the much-hyped Stupp paper in late 2021, see her full report here. Said Alina, “My default is to roll my eyes when a set of relatives and friends all start sending me the same news blurb for another spinal cord injury study. … It’s rare that a piece of research lives up to the hype that a university press machine is drumming up. But I must admit, the work published by the Samuel Stupp lab . . .does appear promising.”
Matrix + Stem Cells
Ok, now let’s look at the new paper from the Stupp group, “Artificial extracellular matrix scaffolds of mobile molecules enhance maturation of human stem cell derived neurons,” published by Cell Stem Cell, lead author Evangelos Kiskinis, Northwestern School of Medicine.
There is a lot of excitement about iPSCs. They are very similar to an embryonic stem cell in their ability to self-renew and differentiate into any other cell type – minus ethical baggage. Because they derive from one’s own body they don’t get destroyed by the immune system. The potential for therapies is high, and iPSCs are very important in disease modeling and drug discovery.
For a bit of a dive into the iPSC realm, here’s a piece from the journal Nature: How iPS Cells Changed the World, featuring the Nobel Prize winning work of Shinya Yamanaka.
Kiskinis and his team took a human skin cell and using specific transcription factors, reverted the cell into a pluripotent state; they then cultivated the cells to become neurons. They began with the knowledge that iPSCs are problematic when introduced in vitro (in a dish). They don’t mature properly and lack long term vitality. The microenvironment in the body does not nurture their survival. So how about changing the conditions?
From the paper:
To develop more physiological culture conditions, it is important to recapitulate the resident microenvironment of the nervous system. A critical and often overlooked component of this microenvironment is the extracellular matrix (ECM), which plays a pivotal role in neuronal maturation, signaling, and aging.
This is where the Stupp research comes in, using his synthetic biomaterials to introduce polymer scaffolds to mimic the biochemical and mechanical properties of the ECM. The nano-scaffolds, which “dance” and can be tuned in the same way as the ones Stupp reported in the mouse study, encouraged the stem cells to grow and develop.
From the paper:
We report on the use of three artificial ECMs based on peptide amphiphile (PA) supramolecular nanofibers. All nanofibers display the laminin-derived IKVAV signal on their surface but differ in the nature of their non-bioactive domains …. Proteomic, biochemical, and functional assays reveal that highly mobile PA scaffolds caused enhanced b1-integrin pathway activation, reduced aggregation, increased arborization, and matured electrophysiological activity of neurons.
Once again, this is far from being relevant to human application. But it opens up intriguing possibilities for future studies. Per the Kinkinis paper, this “represents a breakthrough in the molecular engineering of artificial ECM scaffolds.”
So enjoy this CureCast, again. Keep your curiosity sharp and your expectations in check. But imagine the future of therapy delivery as a combination of chemistry, materials science, bioengineering, and medicine. This kind of integrated approach has a huge upside; there is much work to do, of course. But a new era of personalized therapy development may be around the corner.